I remember the life-and-death confrontation as if it happened yesterday.
An oncologist was trying to deliver painful news to the son of a grievously ill cancer patient.
“Your mother is actively dying,” the physician said. “I’m not sure if there is a benefit to further aggressive treatment.”
The son shot back: “You must! My rabbi left clear instructions for me to make sure we do everything possible at all costs.”
The doctor explained that resuscitating the dying woman would only cause her more suffering and would be medically and ethically inappropriate. The son would not listen. He stood up, face to face with the doctor, and said, “You will resuscitate my mother or I will grab your hands and force you to!”
I recount this story to highlight an all-too-common experience with well-intended clergy members who become involved in medical care, often without fully understanding the implications of their religious or spiritual guidance. This tension was underscored by a fascinating new study in The Journal of the American Medical Association (JAMA). It found that terminally ill patients who frequently turned to their religious communities for spiritual support were more likely to pursue aggressive medical interventions at the end of life regardless of the medical appropriateness of the care. These patients also were more likely to die in an ICU and less likely to receive hospice care.
On the other hand, the study revealed that end-of-life discussions and the provision of spiritual care by medical teams (including doctors, nurses and chaplains) resulted in less aggressive interventions at the end of life, reducing suffering for patients nearing death.
These results warrant discussion. The study’s authors conjecture that support from clergy members in the community can result in such intense treatment because they may not clearly understand biomedical realities. Well-meaning clergy also may hold firm to a belief in miracles, or focus on the sanctity of life, hope and perseverance even as patients endure the most severe suffering.
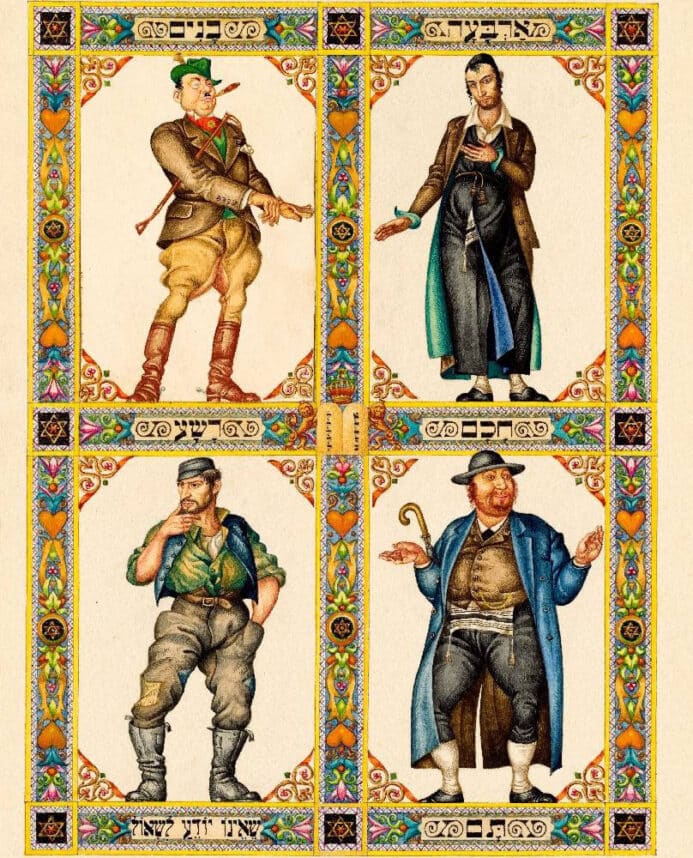
Spiritual care providers in hospitals frequently advocate on behalf of the infinite value of the lives of the terminally ill and often defend decisions to pursue treatment that may be called “futile.” Judaism, as I see it, obligates us to do everything possible to prolong life. At the same time, it encourages us — out of respect for the sanctity of human life — not to prolong the dying process for a terminal patient who does not want to suffer. We must keep people alive as long as we can unless it is counterbalanced by extreme pain and suffering, at which point Jewish law permits a compassionate response of allowing (but not causing) the death process to occur with appropriate palliative care. This was the ruling of Rav Moshe Feinstein, widely regarded as a leading 20th century authority on Jewish law. Our challenge is to determine when a patient’s treatment has gone from life prolonging to dying prolonging. These decisions are often further complicated by some distrustful clergy who take an “us versus them” attitude toward medical professionals.
As a rabbi, I appreciate the incredible importance of hope. It gives people the courage to confront challenging circumstances, and can even alter neurochemistry, significantly aiding the healing process. At the same time, as a chaplain working in a hospital, I see how false expectations and excessive irrational optimism can result in unnecessary suffering, self-blame, and leave people unprepared for adversity.
This is not to say that less aggressive intervention is always ideal, but it turns out that medical professionals aren’t simply trying to save time and money when they counsel against aggressive treatment at the end of life. We know from many studies that physicians themselves are more likely to avoid aggressive treatment and “heroic measures” before they die than are members of the public.
People who work in hospitals know that CPR is rarely as effective at saving the lives of critically ill patients as may be portrayed on prime-time television, and that it can often be a very traumatic experience that does more harm than good.
Hospital chaplains are attuned to the complicated medical realities at the end of life and are thus essential partners in the decision-making process for patients who value religious input.
The delicate balancing act between prolonging life and prolonging dying underscores why people should talk to their families and clergy about their medical wishes at the end of life, and put those wishes in writing by completing advance directives or living wills. The JAMA study highlights the absolute necessity for hospital personnel to reach out to community clergy to better collaborate through open and educational dialogue. That’s what we are hoping to facilitate at my hospital, Cedars-Sinai, in the coming year. As we strive to “choose life,” we recognize that, as Ecclesiastes tells us, “There is a time for everything under the heaven: a time to be born, and a time to die.”



















 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.