“You should know this was my wife’s idea, since I don’t really care to talk about this.”
The words came from Dr. Daniel Stone of Cedars-Sinai Medical Group as he role-played with Dr. Jonas Green of Cedars-Sinai Medical Care Foundation, but they could have come from any aging individual uncomfortable about end-of-life planning.
The two doctors appeared as part of a training seminar on advance-care planning at Temple Isaiah on June 2. Speaking to 35 members of the congregation and of Temple Emanuel of Beverly Hills, the pair emphasized the importance of end-of-life-planning and advised on how to sensitively approach the topic with others.
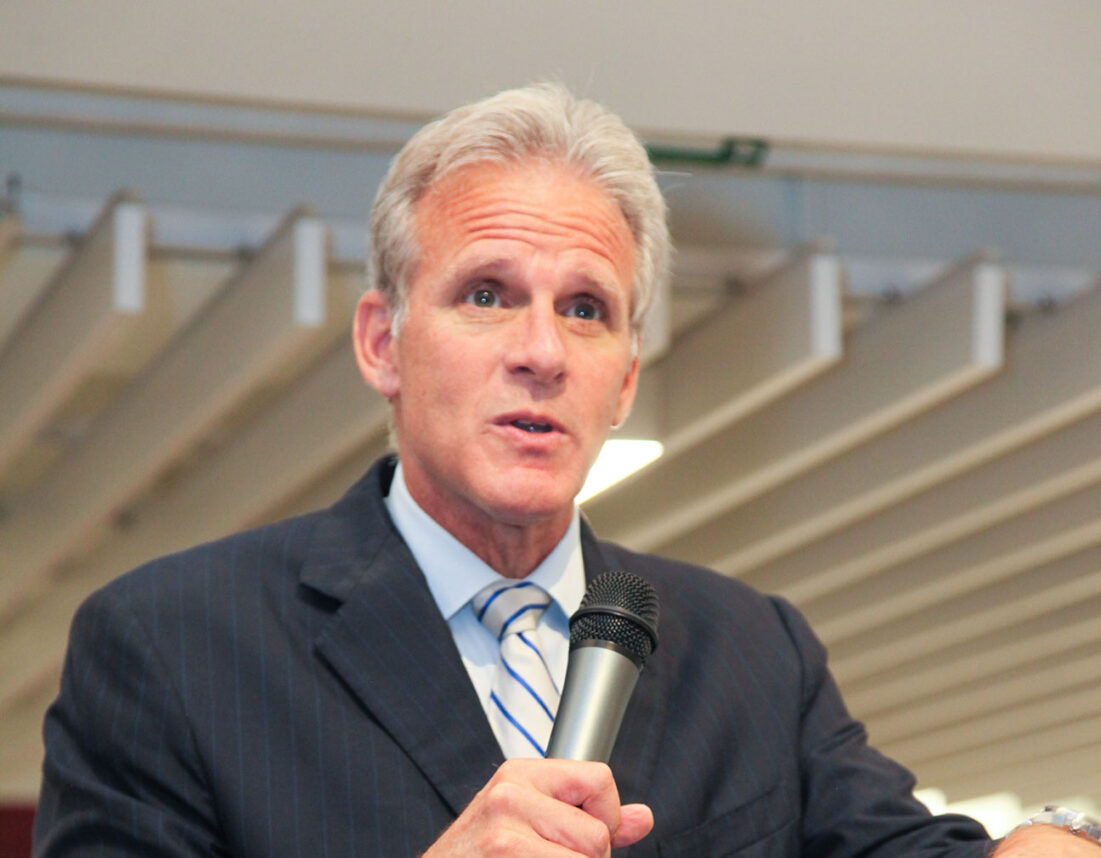
“Historically these conversations only happen when someone is already ill or it’s too late,” said Green, associate medical director for clinical effectiveness at the Cedars-Sinai Medical Care Foundation. “But we hope to make this something people can talk about while they’re healthy and can fully engage in the conversation.”
The training session was a follow-up event to an informational session held on April 28, which was open to the greater Los Angeles Jewish community.
“The goal of this second event is now to train congregants to be facilitators for others to have those conversations,” Rabbi Laura Geller of Temple Emanuel told the Journal. “In Europe, they talk about this in ‘death cafes,’ but I think this is a sacred conversation, which should be taking place in a faith community.”
The two doctors immediately grabbed everyone’s attention as they explained that more than half of all Americans don’t decide how or where they die, although almost everyone says they would like to. They also distributed Cedars-Sinai’s easy-to-understand advance health care directive, one of three steps they discussed to adequately fulfill one’s advance-care planning.
As part of an advance health care directive, one must choose a health care agent — someone to make health care decisions if you are unable to make them for yourself. You should also express your own health care wishes — whether you would like to prolong your life at all costs, for example.
In addition, one should discuss details of one’s end-of-life care (such as whether extraordinary measures should be taken to be kept alive) with loved ones, medical professionals and clergy, and also provide copies of the advance directive to each of these individuals.
As the doctors sat across from each other, they began with examples of how to break the ice.
“I’ve been thinking about my future. Will you help me with something?” Green asked Stone. “I was thinking about a friend of ours’ sudden death, and it made me realize that I always want to be prepared.”
Audience members such as Sheila Wasserman, a member of Temple Emanuel, said the issue hit close to home.
“Facing our mortality can be very frightening, and the more we talk about it, the less frightening these issues become,” she said. “I’m really going to talk with my husband about this now. We’ve done the estate planning, but this is a subject that we’ve danced around.”
As they nibbled on cheese and grapes, attendees asked the doctors about the costs of end-of-life care and how to approach elderly parents, who may be sensitive to the topic. Green said it’s important to remind parents that they can always change their mind about anything; no one needs to feel like they are signing away a right or a responsibility when they make these decisions. And they can plan in as much detail as they like.
Rabbi Zoe Klein of Temple Isaiah brought in a Jewish aspect, handing out packets with prayers and commentaries on them. Titled “A Sacred Conversation,” they included verses from Havdalah, as well as from the Passover haggadah.
“Havdalah is done after Shabbat ends, and it means ‘separation’ — closing a chapter and starting another,” Klein said. “Also, the haggadah is all about conversation, so I thought it would be appropriate to bring it into the discussion. I wanted to put the conversation of death in the context of Jewish rituals. Even though they’re not directly talking about death, I thought it would be appropriate to tie it to something in the Jewish tradition.
“If death was something that most people faced when they were young, there would be a lot of activism about it,” she continued. “But since it’s something that we face when we’re older, we don’t put as much vigor and energy into it.”
Stone, medical director of Cedars-Sinai Medical Group, believes most people avoid the discussion, falling into a don’t-ask, don’t-tell mode that doesn’t help patients
or families.
“Really, most Americans say they want to pass away at home surrounded by loved ones, but the overwhelming majority don’t actually do [this],” he said.
According to The Conversation Project’s national survey on end-of-life conversations in 2013, 90 percent of people say talking with their loved ones about end-of-life-care is important, but only 27 percent have actually done so. Los Angeles, Green said, has one of the lowest rates of Americans with advance-care directives, which led Cedars to host a conference last year to raise awareness of the topic. A follow-up conference is tentatively scheduled to be held at UCLA in May, when doctors may add more of a religious community element, according to Stone.
“I’m hoping we can establish a normative process where we can reach out to other religious institutions,” Stone told the Journal. “With Temple Isaiah and Temple Emanuel, it was a natural partnership, so it seemed like a good place to start.
“Both of them expressed an interest, and they are both progressive institutions involved in the day-to-day lives of their congregants.”
The ultimate goal, according to Geller and Klein, is to reach a point where the synagogues can act as repositories and have advance directives from congregants on hand should doctors need to access it.
Both the doctors and rabbis stressed the importance of encouraging others to plan for the future, while remaining impartial.
“Our goal is to make people come to decisions about the end of their lives, not to encourage them in a particular direction,” Green said. “This issue is a broader one that affects everyone. We hope to see a day where Los Angeles resembles Lacrosse, Wis., where 97 percent of people have completed advance directives. That way, people can live out the last few days of their lives the way they want to.”




















 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.