Usually, the frantic words, “Someone get the rabbi!” uttered in a hospital room mean only one thing. So Debbie Marcus burst into tears when Rabbi Jason Weiner was summoned to her grandfather’s room at Cedars-Sinai Medical Center in July 2008.
Weiner, then interim Jewish chaplain at Cedars-Sinai, quickly assessed the situation: Albert Rubens, 97, had been brought in with a massive heart attack. Although he was still lucid, it was clear he was not going to make it.
But even with that devastating news, the rabbi detected that Debbie’s tears were about something more. And he was right. Albert, known to his family as Pop-Pop, had been eager to see Debbie, then 39, get married, but she and her then-fiancé, Marty Marcus, had not set a date for the wedding.
So someone floated an idea: Get married. Right now.
Did you enjoy this article?
You'll love our roundtable.
Editor's Picks



What Ever Happened to the LA Times?

Who Are the Jews On Joe Biden’s Cabinet?


No Labels: The Group Fighting for the Political Center
Latest Articles

Israel War Room Launches in Spanish
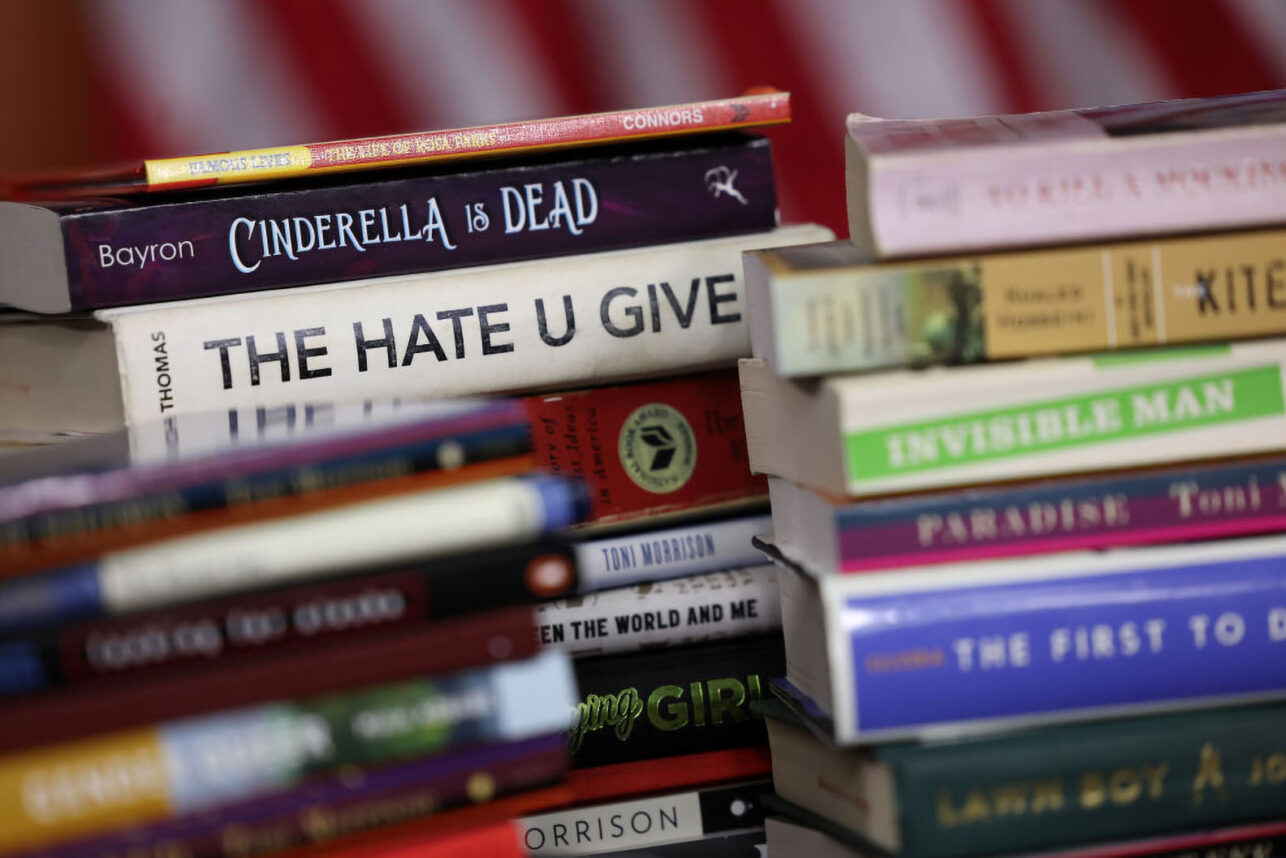
Modern Book Bans Echo Past Atrocities and Further Silence Marginalized Voices

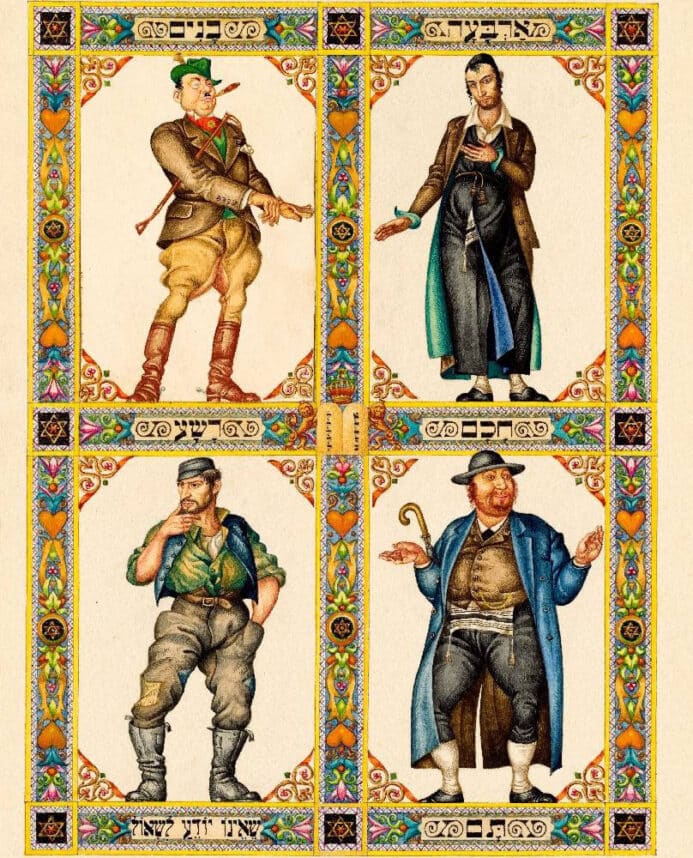
The Power of the Passover Seder to Unite Jews
Dr. Nicole Saphier Reflects on Motherhood and Jewish Advocacy

Israel’s David Moment










 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.